1. What is “cost-effectiveness”?
Cost-effectiveness is a term that is used extensively. Let us consider its meaning in depth.
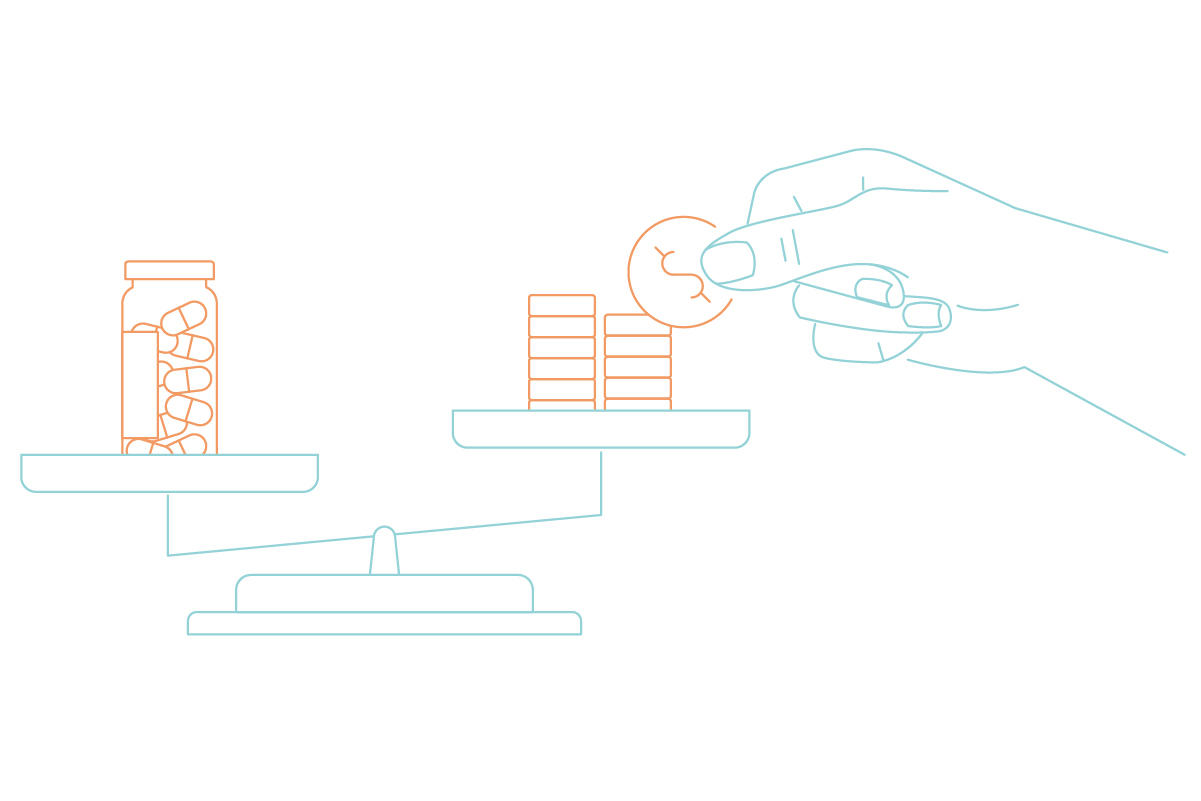
When discussing cost-effectiveness, the balance between the “cost” of treatment and the “outcome” gained is important.
You must have heard of the English proverb, “Pennywise, pound foolish.” Lower cost medicine or medical device is problematic if these are ineffective or of poor quality. Conversely, treatments with a high effectiveness may be beyond the reach of patients (or society) if they are too expensive. What is important is to balance the cost with the outcome. This condition is expressed as “value for money.”
2. Importance of comparisons for cost-effectiveness
There is another important point while considering the cost-effectiveness of healthcare. Cost-effectiveness can be assessed only by comparison with other treatment.
For example, when we state that “you can arrive at the destination earlier if you take a limited express train,” the judgment “earlier” is possible, because the time of arrival is compared with that of a local train. If only limited express trains were available in this world, we cannot judge whether or not taking such trains would allow one to arrive at the destination earlier. You can understand the extent of rapidness only if the statement includes a comparison such as “this train will arrive at Tokyo Station 20 minutes earlier than the local train.”
The same can be said of the cost-effectiveness of healthcare. In this case, the treatment that are used as controls are called “comparator.” Cost-effectiveness cannot be calculated without a comparator. Cost-effectiveness can be determined only in relation to other treeatment.
3. Methods of calculation of the cost-effectiveness
In the preceding sections, we considered the premises needed for discussions about cost-effectiveness.
- Balance between the cost and outcome is important.
- Cost-effectiveness can be determined by comparison with the other treatment.
On the basis of the premises described above, let us try to calculate the cost-effectiveness of healthcare technologies now. This calculation uses the indicator called “incremental cost-effectiveness ratio (ICER),” and employs the equation given below.
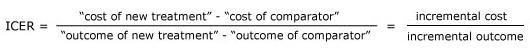
In this equation, the “incremental cost” needed for the use of a new treatment is divided by the “incremental outcome” obtained from the use of the new treatment.
For example, if a new treatment method extends survival by two years compared with the comparator and costs an additional 4 million yen, the calculation would be JPY 4 million ÷ 2 life-years = JPY 2 million/life-year gained. This is interpreted as “requiring an additional JPY 2 million for gaining one year of survival.” In other words, the cost-effectiveness of a new treatment improves as its ICER decreases.
In the cost-effectiveness analysis, calculation of the ICER is the final goal in many cases. The acceptability of cost-effectiveness is evaluated with the ICER.
Such an attempt has been made not only in Japanese government, but also in other countries. In some foreign countries, cost-effectiveness has been adopted as an element of health technology assessment (HTA). The MHLW calls assessment of the cost-effectiveness of medicines and medical devices “cost-effectiveness evaluation.” It is not an academic term, but we use it if needed.